Rural residents are more prone to chronic pain and opioid addiction, but their health care systems offer fewer alternatives and treatments. In the village of Necedah, population 916, one doctor set out to change that.
Dr. Angela Gatzke-Plamann didn’t grasp the full extent of her community’s opioid crisis until one desperate patient called on a Friday afternoon in 2016.
“He was in complete crisis because he was admitting to me that he had lost control of his use of opioids,” recalls Gatzke-Plamann, 40, the only full-time family physician in the central Wisconsin village of Necedah, population 916, nestled among bluffs and pines.
The patient had used opioids for several years for what Gatzke-Plamann calls “a very painful condition.” But a urine screening one week earlier had revealed heroin and morphine in his system as well. He denied any misuse that day. Now he was not only admitting it, but asking for help.
But Gatzke-Plamann had no resources to offer. Both she and the patient started searching the internet while still on the phone, trying to find somewhere nearby that could help. No luck. Here was a patient with a family and job who spiraled into addiction due to doctor-prescribed pain pills, yet the community’s barebones health system left him on his own to find treatment — which he later did, 65 miles away. If that situation was going to change in Necedah, it was up to Gatzke-Plamann to change it.
“That weekend I went home and I said, ‘I’ve got to do something different,’ ” Gatzke-Plamann recalls.
In many ways, rural communities like Necedah have become the face of the nation’s opioid epidemic. Drug overdose deaths are more common in rural areas than in urban ones. And rural doctors prescribe opioids more often by far, despite a nationwide decline in prescribing rates since 2012.
Meanwhile, rural Americans have fewer alternatives to treat their very real pain, and they disproportionately lack access to effective addiction treatment like the medication buprenorphine. For rural physicians like Gatzke-Plamann, the burden of responding to the opioid epidemic falls on their already-loaded shoulders.
Rural residents report more pain
One reason there are more opioid prescriptions in the rural United States: Those residents report more chronic pain. For one, rural communities skew older, meaning they disproportionately deal with painful conditions related to aging, such as arthritis. Injuries also appear to be more common among communities more dependent on jobs that call for physical labor, such as mining and logging.
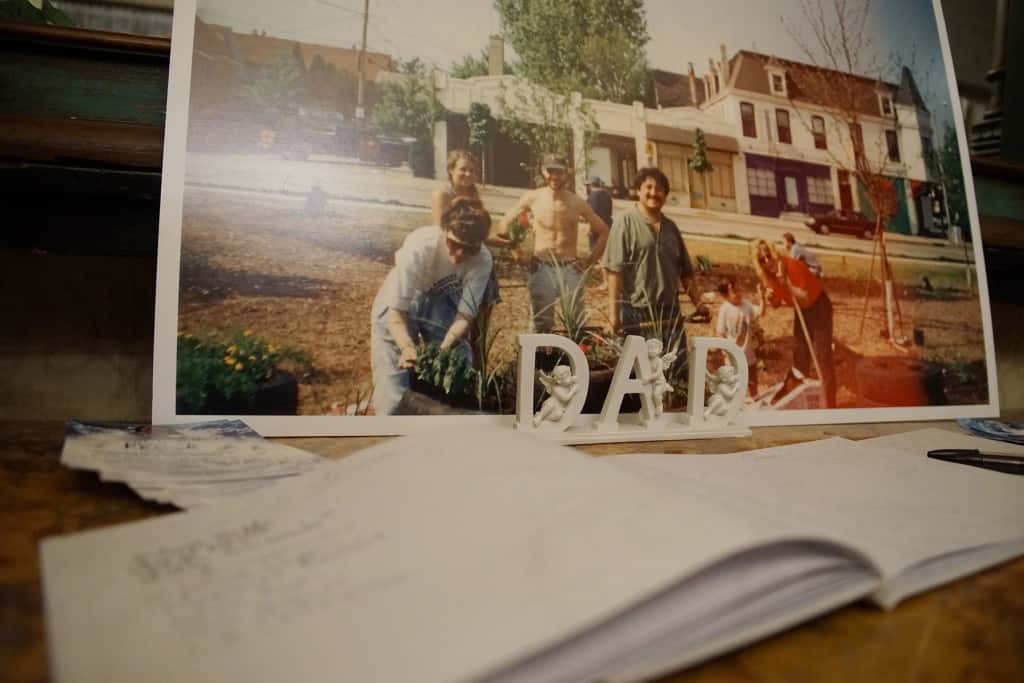
For 62-year-old Necedah resident Michael Kruchten, the chronic pain stems from chemotherapy and radiation therapy treatments he received for lung cancer back in 2011. Kruchten is cancer free now, but the treatments left him with neuropathy — permanent and severe nerve damage — in his hands and feet.
“It’s very hard to explain,” Kruchten says of the pain caused by his neuropathy. “Sometimes it’s a burning — a continuous burning. Sometimes it’s just like a sharp jolt of pain. And then sometimes it’s just pain, pain, pain.”
The pain forced him to stop working at the ethanol plant in Necedah. Daily chores like chopping wood for his furnace or even carrying a plate of food became challenging. And maybe worst of all, the pain would keep him awake a night.
“A lot of nights I pounded the pillow trying to get to sleep, I’d get so frustrated and restless,” Kruchten says.
Gatzke-Plamann tries to avoid prescribing opioids when she can, but alternatives are limited around Necedah. The nearest physical therapy is in Mauston, a 17-mile drive south. Other treatments such as cognitive therapy for pain require an even further drive to Madison, Marshfield or La Crosse, each at least an hour away.
She first tried prescribing Kruchten gabapentin and then duloxetine, two non-opioid medicines for treating pain. Neither helped enough. Eventually she prescribed the opioid hydrocodone, two pills before bed in the evening. That finally gave Kruchten enough relief to sleep.
“Without the sleep I was a couch potato,” Kruchten says. “Once I started to get to sleep (at night), I got rid of my TV and the couch and started becoming more active.”
Doctor launches multi-pronged effort
Necedah is not exactly at the center of the opioid epidemic, but it is not far from it either. The overdose death rate in Juneau County — home to Necedah — tracks with the state average, which itself is about average in the United States. But Juneau County shares a border with Adams County, which has one of the highest overdose death rates in the state.
When Gatzke-Plamann came to Necedah in 2010, U.S. opioid prescriptions were peaking. She estimates she inherited 25 to 30 patients with monthly opioid prescriptions. Soon she, just like her peers around the country, noticed a rise in opioid overdose and misuse.
“We were seeing that some patients were losing control of their ability to use these. It became very problematic,” Gatzke-Plamann says.
Today, Gatzke-Plamann’s affiliated hospital sends her a monthly report of how many of her patients have opioid prescriptions. It varies from month to month, she says, but it is usually between seven and 10. And that is after her concerted effort.
Around 2012, she stopped taking on new patients using chronic opioid medications so she could focus on her current opioid patients. She weaned many of them off of opioids altogether and tracked how many individual pills she prescribed for acute pain. Instead of defaulting to a month’s worth of pills for a C-section patient, for example, she might only prescribe three to five pills.
“Most of the time those patients really only have that much pain for a couple of days,” Gatzke-Plamann says. “We don’t need to have those pain medications sitting in their medicine cabinets.”
Gatzke-Plamann helped shape her community’s wider discussion about opioids. That included joining the county’s substance abuse prevention coalition and addressing her peers about best prescription practices.
Agreements help opioid users
Around 2016, Mile Bluff Medical Center — the hospital in Mauston with which she is affiliated — established a standardized medication treatment agreement, contracts with patients laying out rules for opioid prescriptions.
Patients such as Michael Kruchten must agree to a litany of stipulations before getting a new prescription. That includes getting pills from only one doctor and filling prescriptions at just one pharmacy. Patients must also submit to random pill counts and urine screenings. Kruchten is something of a model patient in that regard, according to Gatzke-Plamann.
“You come in for appointments regularly and you’re always on time and you’re respectful with the staff,” she tells him as they review the contract at an appointment in November.
Gatzke-Plamann can stop prescribing opioids to patients who violate the agreement. But the contracts aim less to punish than to keep communication open. Each time she reviews the contract with a patient — at least once a year for chronic opioid patients — it allows them to revisit the risks and warning signs of addiction.
On his recent visit, Kruchten tells the doctor he only took one hydrocodone pill instead of his usual two the previous night, saying it was “satisfactory” in curbing the pain.
“And that’s good that you don’t take it to just put yourself to sleep,” Gatzke-Plamann responds. “Because it’s not a sleep medicine. You understand that. We’ve talked about that one before.”
“Yep,” Kruchten agrees.
Treatment lacking in rural areas
The Friday call for help in 2016 made Gatzke-Plamann realize Necedah was missing a crucial resource in solving the pain puzzle: addiction treatment.
“We don’t have as many resources here,” Gatzke-Plamann says of Juneau County, one of the poorest and least healthy in the state. “When I see that there’s a need for something, it’s on me to do something about that.”
She says that is what happened with buprenorphine. Experts use buprenorphine to effectively treat addiction, but the medicine is particularly scarce in rural communities. More than 10 million rural Americans — more than one-fifth of the country’s rural population — live in counties without a single clinician licensed to prescribe the drug. (The rural-urban disparity in access has, however, shrunk since 2017.)
In Wisconsin, 18 of 72 counties lack a buprenorphine provider, and 14 of those unserved counties are rural. Today Gatzke-Plamann is one of only two people in Juneau County licensed to prescribe buprenorphine. The other is a physician’s assistant she supervises. They treat about 10 patients in this small part of their practice that kicked off in October 2018.
Adding addiction treatment to a family medicine practice that was “already at capacity” is not easy, Gatzke-Plamann says. But she took on the challenge, seeing the need in her community.
“That’s sort of how it is with family medicine in a rural area,” she says.
Catina Stoflet is among the buprenorphine patients who benefit. Stoflet, now 35, got hooked on prescription opioids as a 16-year-old in 2001, during the first wave of the nation’s opioid epidemic. She started getting kidney stones in high school. She has had more than 200 of the painful obstructions by her count, leading to many surgeries to remove them.
That first prescription was for Tylenol 3, a combination of acetaminophen and the opioid codeine. But doctors soon escalated her to stronger drugs: vicodin, percocet, oxycodone.
“It was right around the time that people didn’t know what (opioids were) doing to you,” Stoflet says.
Stoflet says she spent years in recovery, including from about 2007 to 2014, and participated in Narcotics Anonymous. But she relapsed in 2014, progressing to harder drugs including heroin and methamphetamine. This year she decided to quit for good. Stoflet says her primary care doctor introduced her to Gatzke-Plamann, who had just recently begun prescribing buprenorphine.
Just like Gatzke-Plamann’s opioid patients, her buprenorphine patients must sign contracts laying out terms of treatment, including agreeing to participate in a treatment program. Stoflet works with a counselor and community recovery specialist at the Roche-A-Cri Recovery Center in Friendship, Wisconsin, about 20 miles from Necedah. The center opened in September 2018. Without its additional resources, Gatzke-Plamann says she would not feel comfortable prescribing buprenorphine.
“I am just one part of their treatment plan,” Gatzke-Plamann says. “I prescribe the medication but they need the counseling. They need the psycho-social support. They need the group meetings. All of that happens because the recovery center opened up.”
Stoflet lives about 30 miles from Roche-A-Cri and 40 miles from Gatzke-Plamann’s clinic in Necedah. Even so, Stoflet calls the long, frequent drives for recovery worthwhile.
‘It might be rocky’
At an appointment in early November, for example, Stoflet was nervous about an upcoming surgery that would require her to briefly pause her buprenorphine treatment and go back to opioids for pain. Her check-up allowed her to talk through the angst and walk through the steps with Gatzke-Plamann.
“We would potentially take you off the buprenorphine and do short-acting pain medications around that time,” Gatzke-Plamann says. “The trouble is then, after your acute pain episode from the surgery is no longer as significant — then we need you to stop those pain medicines for at least 24 hours. And then you can start up on your regular buprenorphine dose.”
“So I will be able to go right to the regular dose,” Stoflet says, “and I should be fine?”
“Yes,” Gatzke-Plamann reassures, adding, “it might be rocky.”
“I know it’s going to be —it’s no treat,” Stoflet replies. “…That’s really fine with me. I was just really worried about how we were going to do this.”
Stoflet did end up on opioids briefly after her surgery in late November. Then she resumed her buprenorphine treatment, just like Gatkze-Plamann said she would. December marks seven months on her medication-assisted treatment journey.
The opioid epidemic is too complicated to boil down to grim statistics about overdose deaths or pills prescribed in any given county. Nor can the stories of one or two patients fully describe it. But the crisis is real across central Wisconsin and beyond.
Dr. Angela Gatkze-Plamann knows that because she confronts it every day.
“I couldn’t imagine not doing it, because — then who would?”
Bram Sable-Smith
Coburn Dukehart
The nonprofit Wisconsin Center for Investigative Journalism collaborates with Wisconsin Public Radio, Wisconsin Public Television, other news media and the UW-Madison School of Journalism and Mass Communication. All works created, published, posted or disseminated by the Center do not necessarily reflect the views or opinions of UW-Madison or any of its affiliates.